Frequently Asked Questions

What is a retinal detachment?
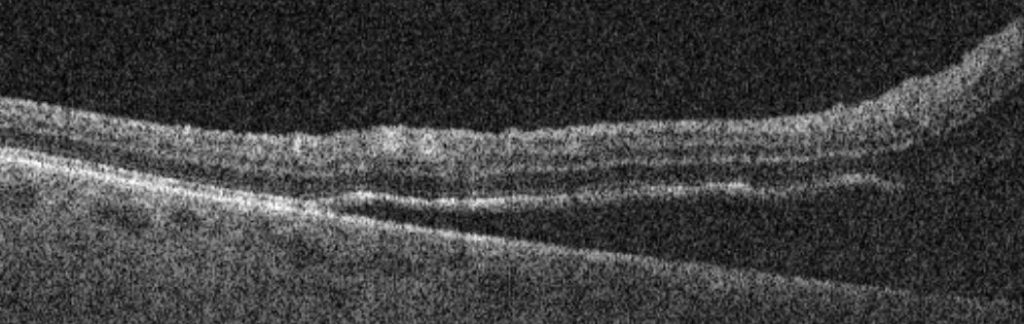
A retinal detachment usually occurs as a result of retinal damage sustained during the process of posterior vitreous detachment (PVD). The retina lines the inside of the eye like a thin wallpaper. A break or hole in the retina can allow the fluid from inside the eye cavity to enter through it and to begin to peel the retina off the wall of the eye. This is called a rhegmatogenous retinal detachment. If a rhegmatogenous retinal detachment is not repaired, it can often cause progressive visual loss and eventually lead to blindness in that eye.
There are other types of retinal detachment, which occur less commonly. Sometimes, thinning at the retinal edges and peripheral retinal round holes can cause very slowly progressive or stable retinal detachments. Pulling forces on the retina due to scarring from any cause can cause tractional retinal detachments – these may also remain stable and not require any intervention. Intra-ocular inflammation can produce exudative retinal detachments, which are treated medically rather than with an operation.
To establish which type of retinal detachment you have and advise on the best treatment, it is imperative to see a vitreoretinal surgeon, who will explain the best approach in your case.
What are the symptoms of a retinal detachment?
Patients will often notice a shadow in the vision, which comes in from the side towards the centre of the vision and looks blurry or dark. Sometimes, a shadow is not seen, and the whole vision is perceived as being blurred. In some cases, only floaters or flashing lights are appreciated, or no symptoms at all!
Because it is impossible to rule out a retinal detachment based on symptoms alone, any change in vision or new onset of floaters or flashing lights should prompt an urgent examination by a qualified eye specialist.
What is the treatment for retinal detachment?
If a retinal detachment has developed, you may rarely be offered observation or laser treatment if this is appropriate in your case, although the usual treatment is surgery. Three general types of operation are available: the vitrectomy, retinopexy and tamponade procedure and the cryotherapy and scleral buckle procedure and the pneumatic retinopexy
Vitrectomy
A vitrectomy, retinopexy and tamponade operation takes between 30 minutes – 2 hours depending on complexity and is usually done as a day case procedure. You will have some eye drops put in before surgery in order to dilate the pupils. A local anaesthetic will be administered, usually in the form of an injection of anaesthetic next to the eye. A mild sedative may be administered to allow you to feel more relaxed. We ask you to lie down on a bed and ensure that you are comfortable for the procedure. The area around the eye will be cleaned with an antiseptic solution and a tented cover placed over half of the face to ensure cleanliness and comfort.
During the surgery, a keyhole approach is used to gain access to the eye. We will remove the jelly from inside the eye to gain access to the retina. Any areas of retinal damage will be identified and treated. The retina will be flattened back into its normal position and a gas bubble will be left in the eye to serve as a tamponade, supporting the retina in position and excluding fluid from the areas of retinal damage as it heals. Sometimes, we will need to use a bubble of special silicone oil instead of gas.
After surgery, it is necessary to use regular eye drops for several weeks to control inflammation and help prevent infection. We ask you to use a plastic protective shield around the eye at night time for a couple of weeks to prevent accidental injury. We may ask you to posture after the surgery. This means he may need to assume a special position, usually looking down at the ground or lying down on one side for several hours or days after surgery. It is possible to take short breaks, however maintaining this positioning improves the chances of retina re-attachment and so it is helpful to do this if you are able.
After surgery, the vision remains very blurred while the gas or silicone oil bubble is present. A gas bubble will slowly disappear over the space of several weeks and your vision should return. An oil bubble persists in the eye until it is removed surgically at a later date. It is important to note that the vision may not be entirely normal and will take several months to continue to improve.
Most operations proceed very smoothly, however sometimes if some other eye conditions or complicating features are present, the operation time and/or the recovery can be prolonged. If this applies to you, the surgeon will discuss it with you before and after your operation and answer any questions you may have.
Cryotherapy and scleral buckle
A cryotherapy and scleral buckle operation takes between 1 – 2 hours depending on complexity and is usually done as a day case procedure. You will have some eye drops put in before surgery in order to dilate the pupils. It is usually done under general anaesthetic, with you being alseep for the surgery.
During the surgery, we will find and treat any areas of damage in the retina and position a silicone implant on the outside of the eye to support the retina as it heals. This implant is not visible post-operatively and can safely remain in position for life.
After surgery, it is necessary to use regular eye drops for several weeks to control inflammation and help prevent infection. The eye may be a little uncomfortable and the drops will help to ease this. We ask you to use a plastic protective shield around the eye at night time for a couple of weeks to prevent accidental injury.
After surgery, the vision remains blurred while the eye heals. Double vision is common for the first few weeks. It is important to note that the vision may not be entirely normal and will take several months to continue to improve.
Pneumatic retinopexy
This procedure is less involved than the other two approaches and can sometimes be performed in a clinic setting. Numbing drops are firstly instilled in the eye to ensure comfort. An examination of the retina is carried out using a head-mounted indirect ophthalmoscope, a piece of special equipment with an attached light source. Any damaged parts of the retina are treated with laser or freezing therapy and a bubble of gas is injected inside the eye to promote the retina to attach.
After surgery, the vision may be very blurred while the gas bubble is present. The gas bubble will slowly disappear over the space of several weeks and your vision should return.
This approach is not suitable for many retinal detachments and very close monitoring is required over the days following the injection, in order to spot problems. If the retina fails to attach using this treatment, repeat treatment or one of the other procedures may be required.
What is the success of retinal detachment surgery?
Overall, over 90% of retinal detachments can be fixed permanently with one operation. One in ten patients will experience a recurrent retinal detachment, which may need further surgery to fix.
