Frequently Asked Questions
What is a diabetic retinopathy?
In diabetes, concentrations of sugar in the blood are raised. Over time, this can damage the smallest blood vessels in your body. The eye has many small blood vessels and the earliest effects of diabetes can often be spotted during a slit-lamp microscopic examination of the retina. In the early stages, these can simply be monitored. This is often done through the diabetic screening programme in the UK.
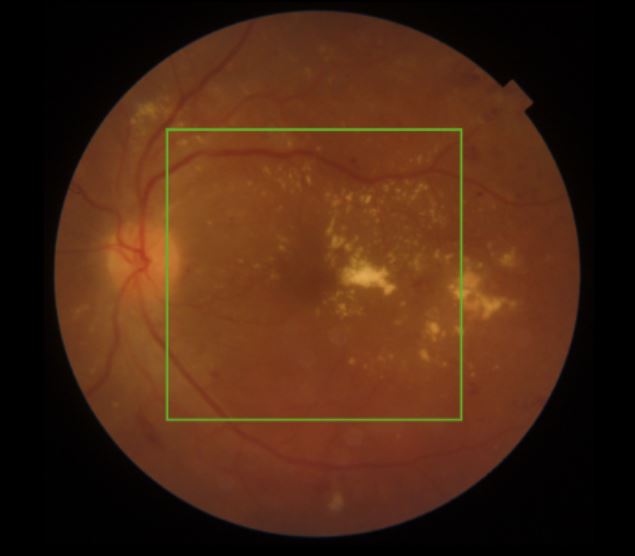
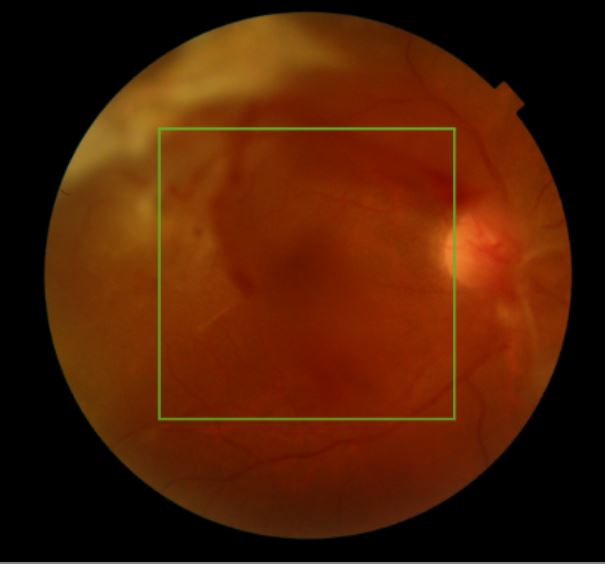
Early changes include retinal microaneurysms (dilated blood vessels) and small retinal haemorrhages (bleeds). As the condition advances, more haemorrhages appear, as well as increasing signs of impaired retinal blood supply, such as white cotton wool spots (swollen retinal layers) and dilated larger blood vessels. Advanced diabetic eye disease can cause severe bleeding in the retina and vitreous. Abnormal blood vessels can be seen to form in the retina and these lead to a number of problems including retinal scarring, epiretinal membranes and retinal detachment.
Other problems can also sometimes develop in the eye alongside diabetic retinopathy, such as a special form of glaucoma (optic nerve damage) called neovascular glaucoma, which may require separate specialist treatment.
What can be done to treat diabetic retinopathy?
Early changes can be controlled and sometimes reversed through maintaining good blood sugar levels, as well as control of your blood pressure and cholesterol. Moderate diabetic retinal changes may require injection treatment into the eye or laser treatment. The former involves anti-VEGF agents and occasionally steroids. These are designed to target diabetic macular oedema, swelling of the central retina which can commonly develop at this stage and impairs the vision. Laser therapy can complement treatment for diabetic macular oedema. The best approach is very individual and a full eye examination and OCT scan is necessary to decide on optimum management.
For severe diabetic eye disease, pan retinal photocoagulation laser treatment is often required. This involves extensive retinal laser treatment in order to reduce the growth of abnormal blood vessels. Intravitreal injections may also be recommended and occasionally a surgical approach is necessary. An operation for diabetic retinal problems is called a vitrectomy and delamination.
What happens in diabetic eye surgery?
A vitrectomy and delamination procedure takes anywhere from 30 minutes to 2 hours, depending on complexity. It is usually done as a day case procedure. You will have some eye drops put in before surgery in order to dilate the pupils. A local anaesthetic will be administered, usually in the form of an injection of anaesthetic next to the eye. A mild sedative may be administered to allow you to feel more relaxed. We ask you to lie down on a bed and ensure that you are comfortable for the procedure. The area around the eye will be cleaned with an antiseptic solution and a tented cover placed over half of the face to ensure cleanliness and comfort.
A keyhole approach is used and fine instruments are employed to remove the vitreous jelly and any blood from the eye cavity. Scar tissue is carefully removed from the retina and any retinal detachment are identified and treated. Laser treatment is often used at the end of surgery to reduce the chances of further bleeding. After surgery, a bubble of air or gas is usually left in the eye and the vision remains blurred until this disperses. The vision begins to come back from a few days to a few weeks after surgery and may initially remain hazy, as some residual bleeding is common in the immediate postsurgical period. This should clear up over the first few weeks.
After surgery, it is necessary to use regular eye drops for several weeks to control inflammation and help prevent infection. We ask you to use a plastic protective shield around the eye at night time for a couple of weeks to prevent accidental injury.
Most operations proceed very smoothly, however sometimes if some other eye conditions or complicating features are present, the operation time and/or the recovery can be prolonged. If this applies to you, the surgeon will discuss it with you before and after your operation and answer any questions you may have.
What will my vision be like after surgery?
It is important to appreciate that surgery is not a definitive treatment for diabetic eye disease. It is possible that some level of visual impairment will remain afterwards and you may require further treatment with laser, intra-ocular injection or further surgery. For this reason, it is important to continue regular monitoring after having an operation, just as you were doing before surgery.
What is diabetic maculopathy?
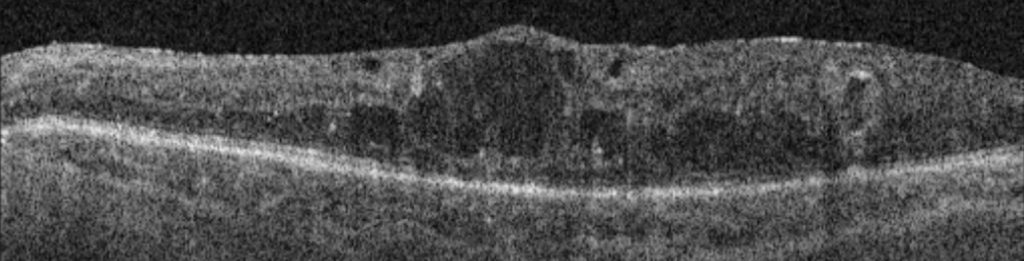
Impaired blood supply to the retina in patients with diabetes can result in problems with the normal function of the retina and sometimes swelling of the central retinal area, the macula (diabetic macular oedema, DMO). On an OCT scan of the retina, you can see increasing retinal thickness and many fluid-filled cystic spaces. This causes a reduction in vision which, if left untreated, can become permanent.
What is the treatment for diabetic macular oedema (DMO)?
The mainstay of treatment for DMO is injections into the eye of an anti-VEGF medication, which reduces the amount of leakage from abnormal retinal blood vessels and helps to reduce the swelling in the macula.
Other treatments which can be used in addition to this include laser treatment and injections of steroids.
