Frequently Asked Questions
What are floaters?
The eye is filled with a clear, jelly-like substance called the vitreous. This is not just made of water, but has protein strands forming a meshwork throughout. This vitreous jelly is not thought to serve any significant purpose in the eye after we are born.
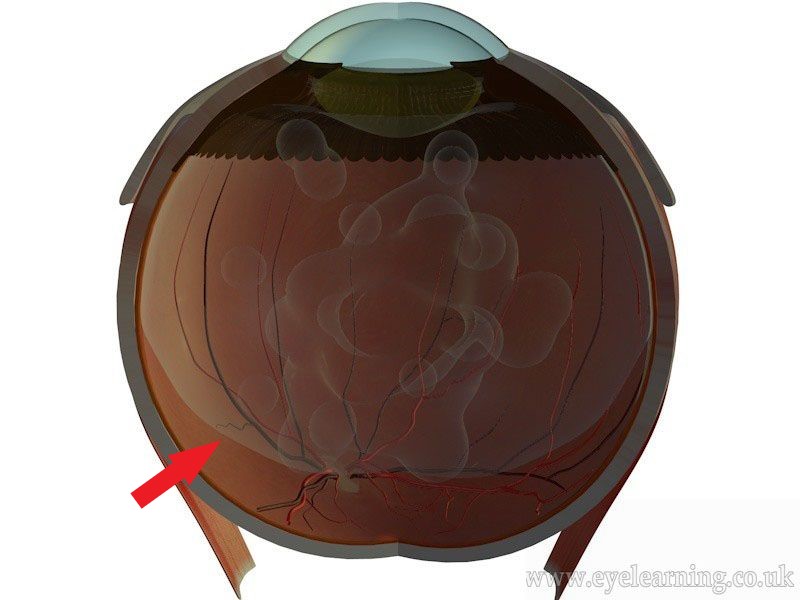
Gradually throughout life, the vitreous softens and degenerates in a process known as vitreous sinuresis. Protein strands in the jelly begin to stick together and can to cast shadows on the retina, appearing as floaters. Eventually, the vitreous jelly softens enough to detach from its position closely opposed to the retina and begins to move around inside the eye (red arrow). This process of jelly detachment is known as posterior vitreous detachment or PVD. It can be associated with a sudden increase in floaters and occasionally flashing lights in the eye (photopsia). The flashes occur because of the physical stimulation of the retina by the pull of the jelly.
Other causes of floaters are possible and include the condition called asteroid hyalosis, intra-ocular inflammation and bleeding inside the eye. The sudden appearance of new floaters should always be checked by an eye specialist.
What problems can a PVD cause?
The jelly never completely separates from the retina, it remains firmly attached at the very edges, all the way around the eye. Closer to the edges, it is more firmly stuck and separates from the retina less readily. This means that the process of PVD can sometimes damage the blood vessels which overly the retina, or indeed cause tearing of the retina itself. This is why it is important to have a full retinal examination should you develop symptoms of floaters or flashing lights, as it is otherwise impossible to know whether any retinal damage has occurred.
If a retinal tear has developed, without treatment this can lead to a retinal detachment in about 50% of cases.
What is the treatment for PVD?
Post patients will have a PVD with no associated complications. If no retinal damage is found, no treatment is indicated. Floaters can be expected to persist, though they do settle down at the bottom of the eye with time and your brain learns to ignore them. Flashes of light may also continue intermittently for a time, before reducing in frequency and settling. This process can take several months. If the floaters persist in the centre of your vision and remain very troublesome, a vitrectomy operation may be recommended.
If a retinal break has indeed developed as a result of the PVD, it is important to treat this promptly with laser or cryotherapy retinopexy. These treatments help reduce the risk of developing a retinal detachment, which can happen as a result of the retinal damage. Laser treatment can usually be carried out in clinic the same day and dramatically reduces the risk of retinal detachment.
What happens during a vitrectomy?
A vitrectomy procedure may be offered for persistent floaters. It takes around from 30 minutes and is done as a day case procedure. You will have some eye drops put in before surgery in order to dilate the pupils. A local anaesthetic will be administered, usually in the form of an injection of anaesthetic next to the eye. A mild sedative may be administered to allow you to feel more relaxed. We ask you to lie down on a bed and ensure that you are comfortable for the procedure. The area around the eye will be cleaned with an antiseptic solution and a tented cover placed over half of the face to ensure cleanliness and comfort.
A keyhole approach is used to remove the vitreous jelly inside the eye, together with the floaters and a full retinal examination is performed. After surgery, it is common to leave a bubble of air inside the eye. This will impair your vision for several days while the air bubble is slowly dispersing.
After surgery, it is necessary to use regular eye drops for several weeks to control inflammation and help prevent infection. We ask you to use a plastic protective shield around the eye at night time for a couple of weeks to prevent accidental injury.
Most operations proceed very smoothly, however sometimes if some other eye conditions or complicating features are present, the operation time and/or the recovery can be prolonged. If this applies to you, the surgeon will discuss it with you before and after your operation and answer any questions you may have.
