Frequently Asked Questions
What is a macular hole?
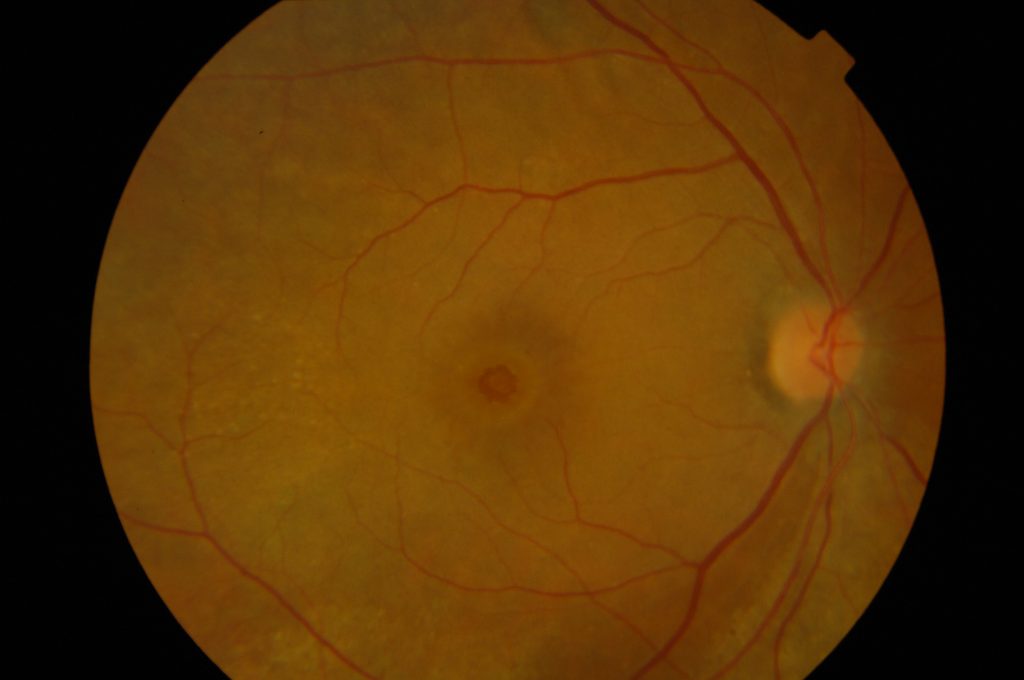
The retina is a thin wallpaper that lines the inside of the eye. It is formed of layers of nerve tissue and act like a film of a camera, picking up the light entering the eye and sending images to the brain. The central part of the retina is called the macula and this is responsible for the sharp vision that allows us to read and recognise faces.
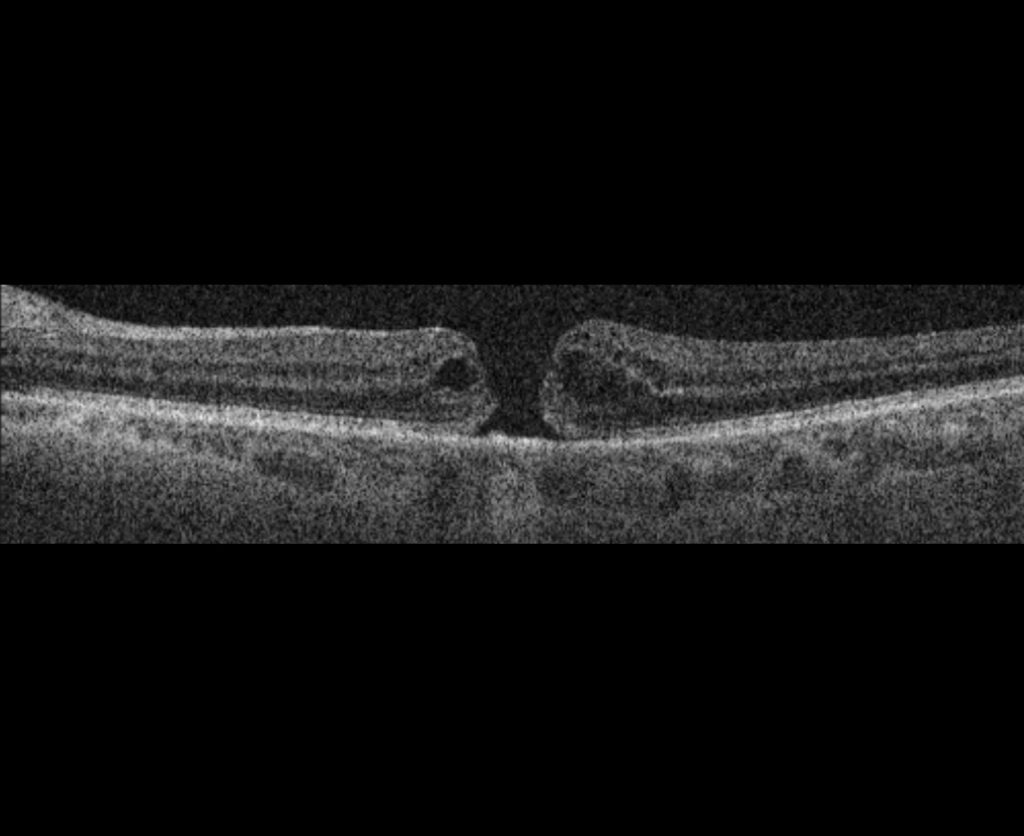
Sometimes, as a result of ageing changes in the eye, a split forms in the retina in this central area. This is called a full thickness macular hole. If the split only involves some of the retinal layers and does not go all the way through, it is called a lamellar macular hole or a lamellar defect. It is important to differentiate full thickness macular holes and lamellar macular holes. The latter are also a result of slow degenerative changes in the retina, however they commonly have a much smaller effect on vision and are generally not amenable to surgery like their fill thickness counterparts.
What problems does a full thickness macular hole cause?
Macular hole formation can cause symptoms of blurring, distortion and “missing” vision. If left untreated, vision can be expected to slowly decline, although you would not lose the vision entirely from this condition. It is likely that things will get quite blurry, to the point where you struggle to see the letter chart at the optician. Your peripheral vision remains unaffected.
Sometimes, these holes may close by themselves, although this is generally only possible in the first few weeks after their formation. If the hole remains open beyond the first month, it is unlikely to close spontaneously.
What treatment is available for macular holes?
The treatment which may be offered for a macular hole is an operation called a vitrectomy, ILM peel and gas. The procedure takes about 1 hour and is usually done as a day case procedure. You will have some eye drops put in before surgery in order to dilate the pupils. A local anaesthetic will be administered, usually in the form of an injection of anaesthetic next to the eye. A mild sedative may be administered to allow you to feel more relaxed. We ask you to lie down on a bed and ensure that you are comfortable for the procedure. The area around the eye will be cleaned with an antiseptic solution and a tented cover placed over half of the face to ensure cleanliness and comfort.
During the surgery, a keyhole approach is used to gain access to the eye. We remove the vitreous jelly from the eye cavity and peel off a thin inner layer of the retina to allow the retina to become more flexible. This helps the edges of the hole to stretch and come together. A bubble of special gas is left in the eye at the end of surgery, which also helps the hole to close.
After surgery, it is necessary to use regular eye drops for several weeks to control inflammation and help prevent infection. We ask you to use a plastic protective shield around the eye at night time for a couple of weeks to prevent accidental injury. We may ask you to posture after the surgery. This means he may need to assume a special position, usually looking down at the ground for several days after surgery. It is possible to take short breaks, however maintaining this face-down positioning improves the chances of hole closure and so it is helpful to do this if you are able.
After surgery, the vision remains very blurred while the gas bubble is present. The gas bubble will slowly disappear over the space of several weeks and your vision should return. It is important to note that the vision will not be entirely normal and will take several months to continue to improve. Overall, over 90% of macular holes can be closed surgically.
Most operations proceed very smoothly, however sometimes if some other eye conditions or complicating features are present, the operation time and/or the recovery can be prolonged. If this applies to you, the surgeon will discuss it with you before and after your operation and answer any questions you may have.
How soon should a macular hole be repaired?
Macular hole surgery should not be delayed. A few extra weeks are not generally thought to make a difference to the visual outcomes, however leaving a macular hole from many months can decrease the chances of hole closure with surgery. It is always best to discuss your specific case with the surgeon to weigh up the particular risks and benefits and in your case.
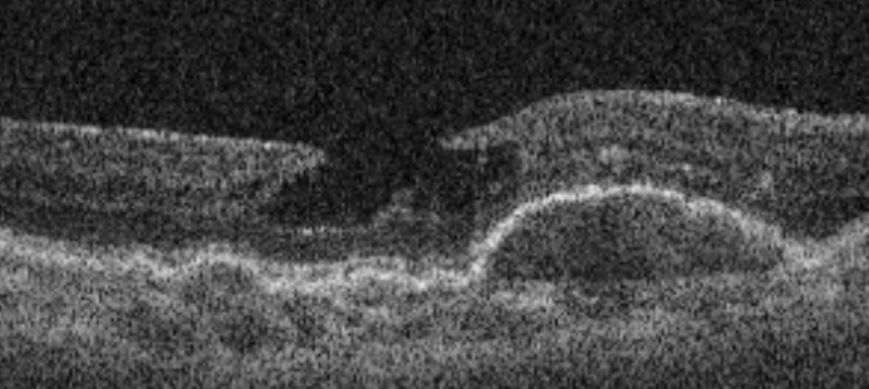
This OCT scan shows a lamellar macular hole. This condition is not usually treated surgically, unless it progresses to a full thickness defect. The vision frequently remains good and, though progression can be noted, is is usually slow and may not cause significant visual problems.
A consultation is advised to review your macular hole and suggest the most suitable strategy.
