Frequently Asked Questions

What is macular degeneration?
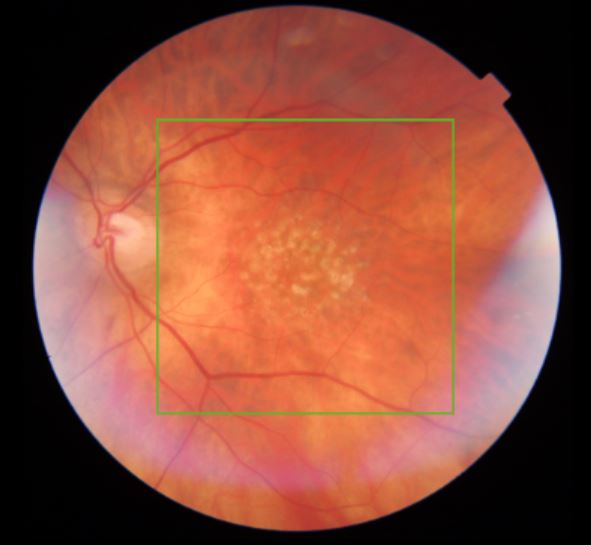
Age-related macular degeneration (AMD) is a condition of the retina that develops to some degree in over 25% or a quarter of all those aged 60 or over. It is “wear and tear” of the retina and can be diagnosed on clinical examination by an optometrist or ophthalmic specialist. There are two broad types, the so-called dry and wet forms. In dry AMD, colour changes are noted in the retinal pigment epithelial layer underneath the central part of the retina, the macula. There can also be drusen, collections of spent retinal cells, which look yellowish and produce a bumpy appearance in the retina on cross-sectional OCT scan of the macula.
Wet or neovascular AMD is a rarer form of the condition, which can develop in a small proportion of those with dry AMD. In this case, there is a disruption in the normal retinal layers and abnormal blood vessels (choroidal neovascular membranes, CNVM) begin to develop underneath the retina. These can cause pockets of fluid to accumulate underneath and within the retina as well as cause bleeding in the macula.
What will happen to my vision if I have AMD?
In the majority of people, AMD will not result in a significant visual problem. Many people do not realise that they have the condition and their visual acuity can remain normal or near-normal.
In the case of dry AMD, vision does slowly decline and so you can expect to notice a few changes after having the condition for a number of years. Symptoms that are frequently reported are distortion of vision and blurring, which is not correctable with glasses. These changes advance very slowly and many people may not even notice the gradual visual decline. This is one of the reasons that regular optician or ophthalmologist checks are recommended, to pick up nay problems early and ensure your vision remains at driving standard.
In cases of wet AMD, similar symptoms of distortion and blurring are reported, however the visual change usually happens more suddenly and is therefore more readily noticed. It is important to have your eyes examined promptly should you ever develop a sudden change in your vision.
Can AMD be treated?
There is no established medical or surgical treatment for dry AMD, however there are many health and lifestyle measures which can help to prevent and slow down the condition. One of the main risk factors of AMD development is smoking, so smoking cessation is recommended. Eating a healthy diet rich in leafy green vegetables ensures a good supply if vitamins and minerals necessary for retinal health. Although a healthy diet provides plenty of nutrients in the majority of people, vitamin supplementation can also be recommended. A series of scientific studies (AREDS and AREDS2) established the vitamin combinations most useful for retinal health and you should check that your vitamin preparation corresponds to this AREDS formulation.
If you develop wet AMD, treatment is available in the form of anti-VEGF agents, which are usually delivered via monthly injections into the eye. Commonly used agents include ranibizumab (Lucentis®) and aflibercept (Eylea®). It is important to be assessed promptly by an ophthalmologist if you are suspected of developing wet AMD, as delay in treatment can result in visual loss. Your suitability for treatment and an individual treatment programme can be worked out and initiated by your specialist.
How do I know if my AMD is getting worse?
It is important to regularly monitor your own vision. Changes are not always immediately apparent and it is helpful to use an Amsler chart. This can be used daily or weekly to more easily pick up any changes in your vision.
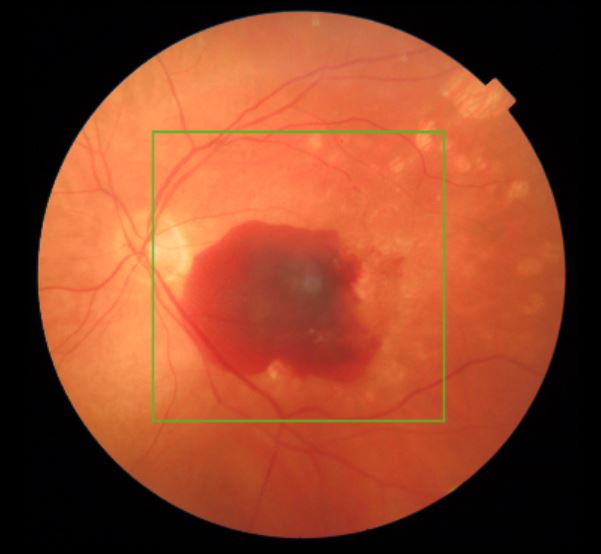
What is sub-macular haemorrhage?
Several processes is in the eye can give rise to bleeding underneath the retina. This most commonly happens as a result of wet macular degeneration, although high myopia (very short sighted eyes), eye inflammation and injury can also cause this. The reason for the bleeding is the formation of abnormal blood vessels in the layers underneath the retina.
The symptoms are usually a fairly sudden onset of blurring and distortion in the central vision. It may happen out of the blue, even if you do not have a diagnosis of any eye problems. If the bleeding occurs in the periphery of the retina, no treatment may be recommended except observation. Bleeding under the macula, however, may require a surgical approach. If nothing is done, the blood forms a fibrous scar over time and the vision is not likely to return to normal.
There are two surgical approaches. The first is recommended in smaller bleeds and involves an injection of special gas and a clot busting agent such as tissue plasminogen activator into the cavity of the eye. The drug attempts to dissolve the blood clot and the gas bubble acts with gravity to help shift the blood away from the central retina. This second approach involves a vitrectomy operation, where keyhole instruments are used to remove the vitreous jelly and deliver that clot busting agent directly underneath the retina to dissolve the blood clot. A gas bubble is left in the eye to encourage the blood to shift away from the macula. In both cases, you will be asked to posture, which means you will need to assume a particular head position, usually looking down at the ground. This will need to be maintained for anywhere between a few hours to a few days after surgery and increase the chances of the blood clot shifting.
These treatments are successful at improving vision in about 50% of cases.
What further support is available?
If you are struggling with your vision, an appointment in a low vision clinic (LVA appointment) can be arranged with a specialist optometrist. It may also be helpful to discuss the possibility of sight impairment registration with your ophthalmologist, which allows more support from your local Council.
There are many organisations which offer help and support to patients. You can find links to some of these below.
