Frequently Asked Questions

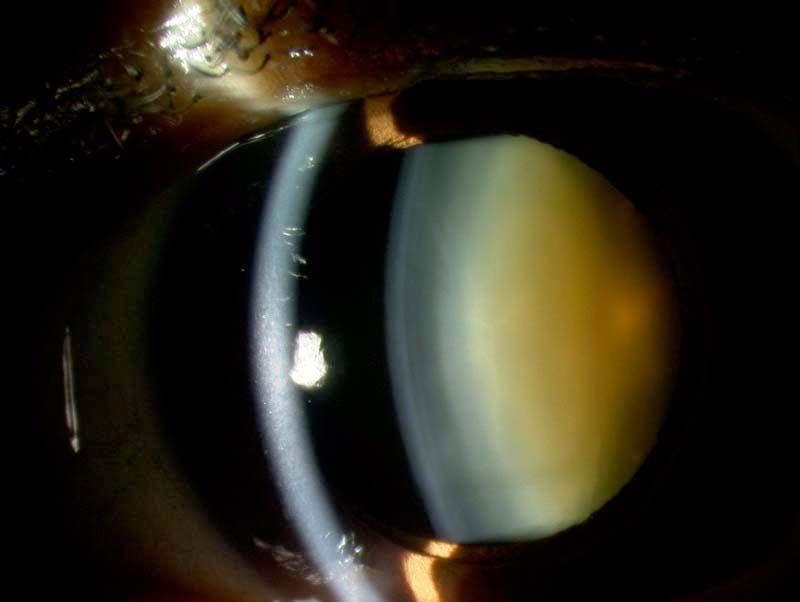
What is a cataract?
A cataract is the clouding of the natural crystalline lens of the eye. The lens is located inside the eye, just behind the iris (coloured part of the eye) and pupil. Over time, the naturally clear lens can become milky or develop areas of clouding. This is the natural consequence of ageing and can be accelerated by many things, including genetic factors, sunlight exposure and previous history of eye inflammation, trauma or surgery.
What will I notice if I have a cataract?
Early lens opacity may not produce many symptoms. Sometimes, patients can notice a paradoxical improvement in vision at certain distances, as an early cataract will change your refraction (glasses prescription). Other early symptoms frequently include glare and haloes, difficulty with night driving and increasing problems with reading small text.
Advancing cataract will usually produce a reduction in visual acuity, increasing difficulties with driving and trouble with all tasks conducted in low light. If driving is important to you, it is vital to monitor your own ability to see a car license plate at 20 metres, which is the UK legal driving vision requirement.
Should I have cataract surgery?
Excepting some special rare cases where a cataract may be causing other problems in the eye, most cataract surgery is optional. It is up to you at which stage cataract surgery is carried out. The timing of surgery will be highly individual and will depend upon your level of vison and the extent of the difficulties which you are having.
For some patients, cataract surgery may be advised at the earliest opportunity, as their occupation or hobbies may cause cataract symptoms to become problematic at an early stage. Other patients may notice few problems from their cataract until it is more advanced. Operating on cataracts carries slightly higher surgical risks if the lens opacity is very advanced, however most people request surgery at a much earlier stage as they begin to experience visual problems.
What is involved in cataract surgery?
A cataract operation (phacoemulsification and intra-ocular lens implant) takes about 20 minutes and is done as a day case procedure. You will have some eye drops put in before surgery in order to dilate the pupils. A local anaesthetic will be administered, usually in the form of drops. Sometimes, an injection of anaesthetic next to the eye is used for longer-lasting numbing effect. We ask you to lie down on a bed and ensure that you are comfortable for the procedure. The area around the eye will be cleaned with an antiseptic solution and a tented cover placed over half of the face to ensure cleanliness and comfort. Using a keyhole approach, small instruments are used to gently remove the cataract using ultrasound energy. A new plastic lens implant is be placed in the eye to focus the light. This surgery is painless, and vision is often restored almost immediately. After surgery, it is necessary to use regular eye drops for several weeks to control inflammation and help prevent infection. We ask you to use a plastic protective shield around the eye at night time for a couple of weeks to prevent accidental injury.
Most operations proceed very smoothly, however sometimes if some other eye conditions or complicating features are present, the operation time and/or the recovery can be prolonged. If this applies to you, the surgeon will discuss it with you before and after your operation and answer any questions you may have.
What will my vision be like after surgery?
Cataract surgery changes the focusing power of the eye. This can be an opportunity to say goodbye to glasses. The most commonly used lens implants focus the light coming from one specific distance. This means that if the implant provides clear distance vision, you will require reading glasses for near work and vice versa. Other types of implants exist which aim to provide spectacle free vision at a greater range of distances. These choices and their benefits and drawbacks will be discussed with you when planning your surgery so that an informed decision can be made about the correct implant for you
